Use of antipsychotics in Maine nursing homes climbs
Sherri Parker, assistant director of nursing at Caribou Rehab and Nursing, recalled a woman who came to her facility and was so sedated by the prescribed antipsychotic medication she had been taking at home that they couldn’t keep her awake for therapy because “she’d fall asleep in front of you.”
Parker, who handles gradual dose reductions at the nursing home, said she worked with a doctor to wean the woman off the medication. By the time the resident transferred back home two months later, “she was a completely different woman,” Parker said — able to eat on her own and be home alone while her husband went to work.
“I’ve seen a stopped antipsychotic medication on many people and sometimes I’m like, ‘Wow, they’ve actually done really well.’ That just goes to show me that it really wasn’t necessary to keep them on that,” Parker said.
But in recent years, she has seen an increase in these medications. At the end of last year, while reading referrals from the hospital for new residents, Parker said nearly every one had a prescription for an antipsychotic medication. She said it’s likely they were prescribed the medication while living at home or when they went to the hospital before ending up at her nursing home.
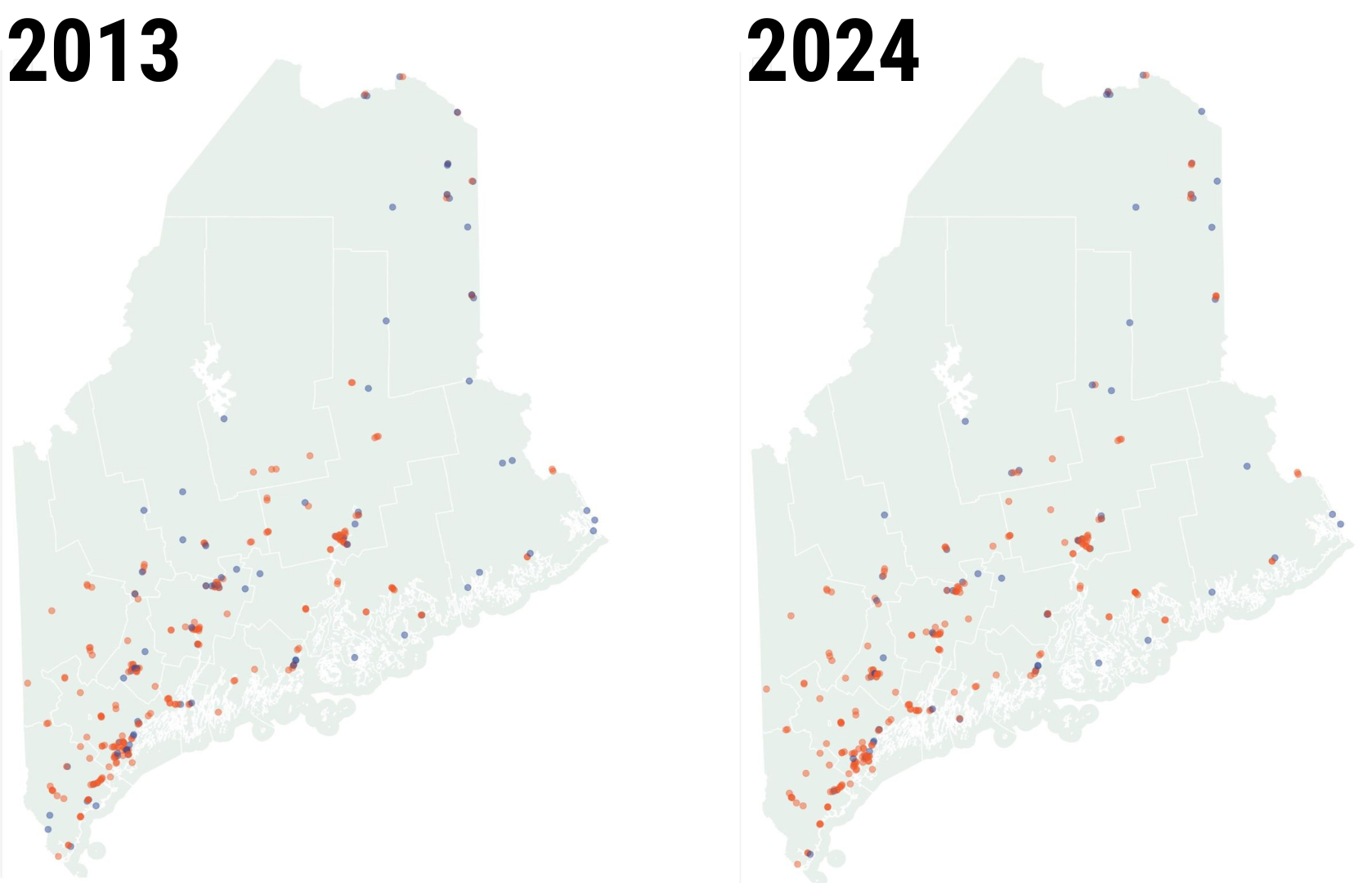
Statewide data shows the percentage of Maine nursing home residents receiving antipsychotic medication is increasing.
While the rate for short-stay residents, like the one Parker recalled, is relatively low, Maine’s rate for long-stay residents is higher than the national average. Short-stay residents are in a nursing home for less than 100 days, often recovering from surgery or being discharged from a hospital, according to the U.S. Centers for Medicare and Medicaid Services.
In the years after federal regulators cracked down on rates of antipsychotic medication given to long-stay nursing home residents, Maine became a success story, dramatically reducing its rate between 2011 and 2017 from 27 to 17 percent.
But since then, Maine’s rate has crept back to 20 percent, higher than the national average of 14.7 percent and the sixth-highest across all states, according to the U.S. Centers for Medicare and Medicaid Services. Among all American adults, the rate of antipsychotics was less than 2 percent.
Antipsychotics are a type of medication, including Risperdal and Seroquel, designed to manage psychosis and delusions. They’re often given to patients with a diagnosis of schizophrenia or bipolar disorder. The side effects can be severe, including tremors, heart and circulatory problems, high cholesterol and sedation. They can be particularly problematic for older adults, even potentially shortening the lives of nursing home residents by increasing the risk of drowsiness, confusion and falling, said several experts.
CMS data on nursing home rates of antipsychotics exclude people diagnosed with schizophrenia, Tourrette’s Syndrome and Huntington’s Disease.
“Antipsychotic medications are especially dangerous among the nursing home population because of their potentially devastating side effects, including death, and the use of antipsychotic medications among nursing home residents is an indicator of nursing home quality,” a CMS spokesperson told The Maine Monitor.
Treating an episode, not a behavior
Dr. Susan Wehry, associate clinical professor at the University of New England in Biddeford and a board-certified geriatric psychiatrist, said there are times when antipsychotic medications are necessary to prevent a resident from harming themselves or others, but those occasions are rare.
“I understand an acute need for using a chemical restraint, but call it what it is: This is not treating a behavior; this is treating an episode of agitation that you can’t figure out how to address another way,” Wehry said. “You’re basically sedating the person.”
Wehry said what is often depicted as challenging behaviors from residents with dementia is actually the resident trying to communicate an unmet need. They may not have the language to say what they want, so rather than sedating the resident, it’s important to find out the cause of their frustration, she said.
Parker, with Caribou Rehab and Nursing, said she’s seen residents come off these medications and become more alert, social and talkative. And sometimes there’s no change in behavior, which she said begs the question why the resident needed to be on the medication in the first place.
As of this month, roughly 19 percent of Caribou Rehab and Nursing residents were on antipsychotics, slightly below the statewide average. Parker recalled when their rates were 5 percent and how proud she was, but said the numbers can fluctuate as admissions come in with pre-existing prescriptions.
“I tried really hard with my antipsychotic numbers to be down, and then just slowly they crept up again as we took admissions,” Parker said. “I would love to see my numbers come down and I know those are some things we have to work on.”
Multiple experts and advocates point to a number of explanations for Maine’s rising statewide average, such as staffing shortages and reliance on temporary agency staffing, diminished attention to the problem, MaineCare underfunding for nursing homes, and the all-consuming nature of the COVID-19 pandemic, which demanded more attention on infection control.
Staff who are overwhelmed with duties or haven’t had time to build relationships with residents may turn to medication rather than spending time on de-escalation techniques when residents have challenging behaviors.
“It’s a disappointment to see the rates have increased because I know we can do better,” said Brenda Gallant, Maine’s long-term care ombudsman who advocates for nursing home residents and their families.
Gallant was part of the coalition in 2012 that led the effort to reduce Maine’s rates of antipsychotics, with Wehry and numerous other advocates, providers and organizations.
Multiple people involved in that effort said the success was due to the commitment of a broad coalition that involved statewide trainings, workshops, mentoring programs, grants for innovative programs like Music and Memory, and resources such as a handbook for providers.
The guidance urged providers to take a holistic approach to treating dementia patients, which included education for family members on the risks associated with the medication, staff training programs that identify specific areas of competency and a collaborative transition process with hospitals.
“Initially, we were leaders,” Gallant said, adding that at one point Maine was ranked the seventh-most improved state in 2016, according to federal data cited at the time by the Maine Partnership to Improve Dementia Care in Nursing Homes.
Nationally, the rates during that time decreased from about 24 percent in 2011 to 14.3 percent in 2019, while Maine’s crept back up. But this data also can lag slightly: the collection period for the current data on this quality measure was Oct. 1, 2022 to Sept. 20, 2023.
“The tip of the iceberg”
In recent years, some experts have become concerned about an overreliance on medication for older adults, including Dr. Jabbar Fazeli, who has served as medical director for multiple nursing homes and assisted living facilities in Maine. He said antipsychotics could be the “tip of the iceberg,” and that facilities also use mood stabilizers and sleeping pills as a way to sedate residents.
Fazeli served as co-chair of the Maine Partnership to Improve Dementia Care in Nursing Homes and has been outspoken about reducing overreliance on medication for older adults. Before the federal government decided to focus on the issue, it was difficult to push back against a “pervasive” culture of using antipsychotic medications, Fazeli said.
Durgin Pines in Kittery, where Fazeli served as medical director for more than a decade until last month, maintained a rate of antipsychotic medication that was always below 5 percent, he said. Currently the facility has a rate of 4.2 percent, according to the Centers for Medicare & Medicaid Services. Fazeli said the success was dependent on a joint effort with the director of nursing, assistant director of nursing and the administrator to try all other options before resorting to an antipsychotic medication.
In recent years, lawmakers and the federal government have also become concerned about nursing homes “erroneously” claiming residents had schizophrenia as a way to “mask the facilities’ true rate of antipsychotic medication use,” the agency said in a release last year. CMS conducted onsite surveys to look at schizophrenia diagnoses and conducted audits of how nursing homes coded these residents.
An oversight organization said this does not appear to be a problem in Maine. The nonprofit that provides quality improvement organization services in New England, Healthcentric Advisors, said it has “thoroughly analyzed” Maine data and determined the state is not seeing an increase in schizophrenia diagnoses.
Fazeli added that in his 26 years in geriatric care, Maine is better than most other states, including those he worked in like Missouri, Massachusetts, Connecticut and New Hampshire.

But after a lot of initial energy in Maine, attention on the issue slowed, especially during the pandemic, Gallant said.
Many said the pandemic was all-consuming for nursing home providers, making it difficult to keep the focus on reducing antipsychotics while keeping up with evolving regulations and caring for residents who were forced to be quarantined.
Wehry, the geriatric psychiatrist, said it was understandable for rates to climb back up in the first months of the pandemic, but “that’s no longer an adequate excuse.” She said a lot of nursing homes reverted back to institution-centric care that forces residents to conform to their environment rather than create an environment that works for them.
“I think it’s broader than just the individual person who’s getting the antipsychotic. I think the culture change, which people worked so hard to introduce, also backslid in the pandemic,” Wehry said.
Ruta Kadonoff, who worked for the national nursing home industry group during the 2012 effort to reduce antipsychotic medication, and traveled across the country providing education on the issue, said Maine’s biggest challenge is workforce shortage.
Staff need adequate training on how to “get inside the world of a person with dementia,” time to work with a resident who is upset or struggling to communicate a need, and support to provide person-centered care that allows them to build relationships with residents. None of that is possible in a facility that is understaffed, has high turnover or relies on temporary agency staffing.
“Until we address that, I don’t think it’s realistic to think we’re going to address other quality issues,” Kadonoff said. “It’s a bandaid to try to address other things without dealing with the underlying fact that we just don’t have the people to provide this care and to do it well.”
Healthcentric Advisors, the quality improvement organization, said it has been meeting with the long-term care ombudsman and the Maine Health Care Association, which represents the state’s nursing homes, about refocusing attention on this issue. They plan to update and reintroduce training modules that condense the most useful tools and resources, which will be rolled out in late fall.
The Maine Department of Health and Human Services said it has identified the increasing use of antipsychotics in nursing facilities and encouraged the stakeholder group to reconvene along with nursing facilities administrators and medical directors. In January, DHHS published a stakeholder group report, Improving Quality in Maine’s Nursing and Residential Care Facilities, and noted that “this metric is likely to be among those tied to reimbursement as part of nursing home payment reform,” spokesperson Lindsay Hammes said.
Gallant, the ombudsman, said it’s important to return attention to this problem “if we want to make progress and get back to the place that we had initially in terms of really being leaders. I think that should always be our goal: to do the very best that we can for residents in our nursing homes.”
[ad number=”1″]
The story Use of antipsychotics in Maine nursing homes climbs appeared first on The Maine Monitor.